AI pediatric cancer prediction is revolutionizing the way we approach the treatment and management of childhood cancers, particularly gliomas. A groundbreaking study conducted by researchers at Harvard has revealed that an advanced AI tool surpasses traditional methods in accurately forecasting the risk of cancer recurrence in young patients. This pivotal research employs innovative techniques like temporal learning, allowing the model to analyze sequences of brain scans over time to improve glioma risk assessment. As pediatric cancer recurrence can be both unpredictable and devastating, leveraging AI in medicine offers new hope for tailoring brain tumor treatment and alleviating the emotional burden on families. The potential of this technology to refine patient outcomes and streamline follow-up processes makes it an exciting development in the field of pediatric oncology.
The emerging field of artificial intelligence in pediatric oncology is leading to significant advancements in predicting childhood cancer outcomes, particularly concerning the likelihood of relapse. Utilizing sophisticated machine learning techniques, researchers are uncovering predictive insights that were previously unattainable through conventional imaging practices. By integrating methodologies such as temporal learning into brain imaging analysis, medical professionals can enhance their understanding of recurrence risks associated with pediatric gliomas. This innovative approach not only promises to refine current brain tumor treatment protocols but also aims to ease the stress experienced by patients and their families during follow-up screenings. The considerable accuracy achieved in these predictive models could redefine care strategies, ultimately improving patient survival rates and quality of life.
The Role of AI in Pediatric Cancer Prediction
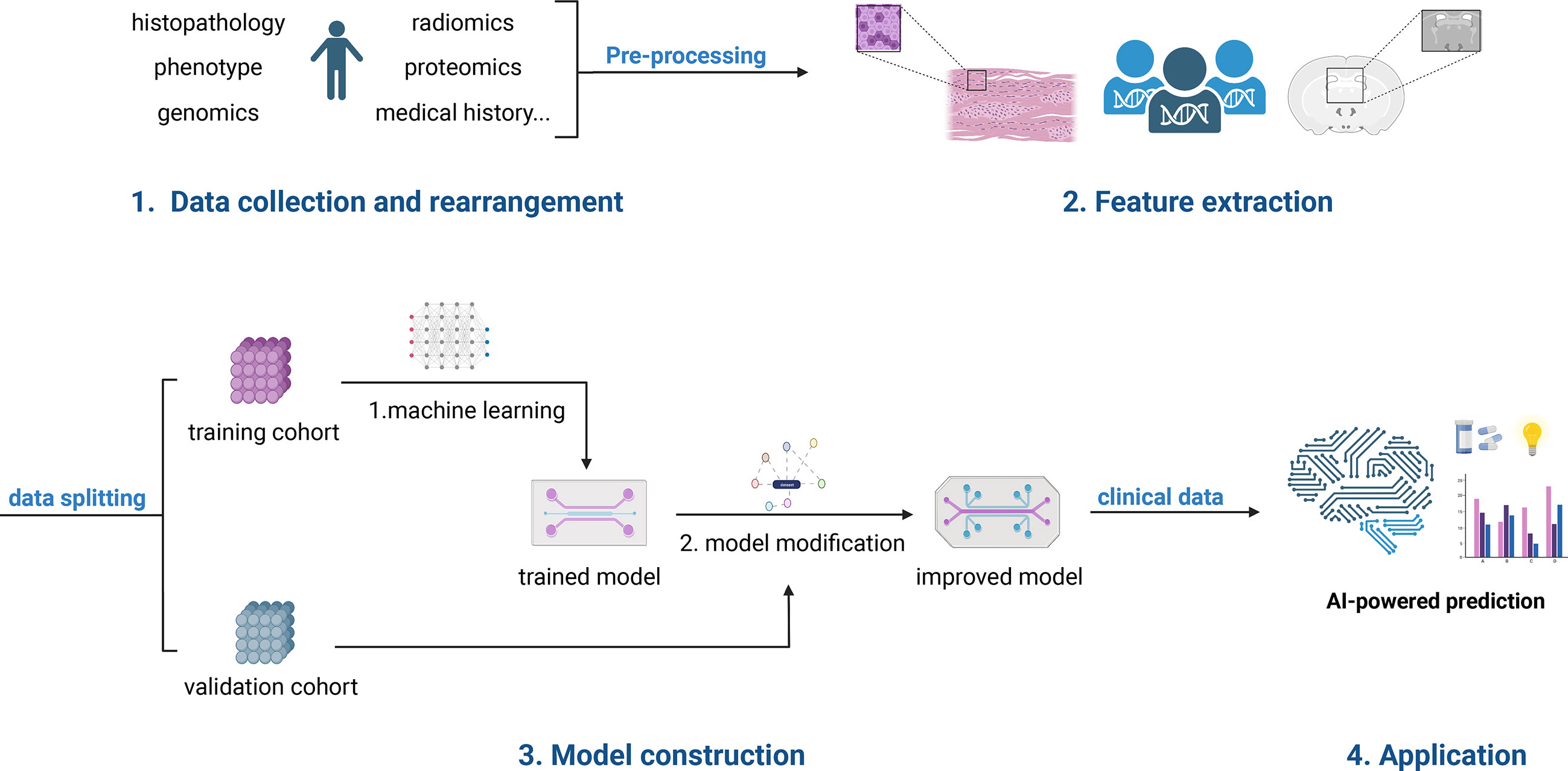
AI has revolutionized the landscape of medical predictive analytics, particularly in the field of pediatric oncology. With an increasing focus on precision medicine, researchers are now employing advanced algorithms to interpret complex medical data. The new AI tool significantly enhances predictive capabilities for pediatric cancer recurrence, offering a fresh perspective on how patients can be monitored post-treatment. This technology builds on traditional imaging techniques, injecting a level of sophistication into diagnostics that was previously unattainable.
Leveraging large datasets, including brain scans from hundreds of pediatric patients, this AI system utilizes temporal learning—a cutting-edge technique that considers multiple timepoints of imaging to make accurate predictions about glioma recurrence. By moving beyond the limitations of analyzing single images, this innovative approach represents a paradigm shift in how medical professionals assess long-term risks in pediatric oncology. As researchers delve deeper into AI in medicine, the potential for improving patient outcomes becomes increasingly apparent.
Understanding Pediatric Cancer Recurrence through Temporal Learning
Temporal learning is a groundbreaking technique gaining traction in the realm of pediatric cancer recurrence assessment. This method allows AI models to synthesize data from sequential MRI scans, making it possible to detect changes that might indicate the onset of a recurrence much earlier than traditional methods could. The findings from the recent study at Mass General Brigham demonstrated the effectiveness of temporal learning in predicting both low- and high-grade gliomas, showcasing an impressive accuracy of up to 89% in post-treatment scenarios.
Integrating temporal learning into the clinical workflow can substantially alter how healthcare providers manage patient follow-ups. Instead of relying on a single MRI’s findings, clinicians can monitor subtle changes over time, reducing anxiety associated with frequent imaging. As this method becomes further validated through clinical trials, it holds potential not only to enhance risk stratification but also to improve treatment strategies, ensuring that high-risk patients receive timely interventions, while low-risk patients can reduce unnecessary imaging.
Advancements in Brain Tumor Treatment with AI
The treatment landscape for brain tumors, particularly pediatric gliomas, is evolving rapidly with the introduction of AI technologies. This transition signifies the potential to tailor therapy more effectively based on a patient’s unique recurrence risk profile. By utilizing AI to predict which patients are at higher risk of experiencing recurrences, healthcare providers can allocate resources more strategically—offering targeted therapies to those who need them most, while allowing others to avoid unnecessary stress over frequent imaging.
Moreover, with AI tools like the one developed by Mass General Brigham, a more personalized approach to brain tumor treatment can be realized. This innovation not only optimizes patient care but also enhances communication between clinicians and families regarding prognosis and ongoing management of pediatric brain tumors. With ongoing research and implementation of these advanced technologies, the future of brain tumor treatment is looking increasingly promising, emphasizing the role AI will play in improving pediatric patient outcomes.
The Importance of Glioma Risk Assessment in Pediatric Patients
Risk assessment for gliomas in pediatric patients is crucial as it informs treatment decisions and ongoing management strategies. Traditional risk assessment methods, which primarily rely on immediate post-operative imaging, lack the depth achieved through temporal learning techniques powered by AI. Enhanced risk assessment not only enables the identification of children who may benefit from closer monitoring but also helps in reducing the treatment burden for those at lower risk for recurrence.
Moreover, understanding the nuances of glioma risk allows clinicians to tailor their approach to follow-up care. With the newly developed AI tools showing considerable promise, more pediatric patients can potentially have their treatment paths optimized based on reliable predictions of recurrence. This dual focus on treatment and risk evaluation is essential for improving the long-term quality of life for young cancer patients and empowering families to navigate an often challenging journey.
AI in Medicine: A New Frontier for Pediatric Oncology
The integration of AI in medicine is paving the way for groundbreaking advancements in pediatric oncology. Researchers at Mass General Brigham have exemplified this through their recent study utilizing AI to predict pediatric cancer recurrence more effectively than previous methodologies. The ability of AI machines to learn from extensive datasets and identify patterns that inform clinical decisions marks a significant milestone in patient care. This represents a shift towards enhanced predictive capabilities in pediatric medicine that could redefine treatment protocols for years to come.
As AI continues to be embraced within clinical settings, the future of pediatric oncology looks promising. It facilitates not only the identification of at-risk children for cancer recurrence but also supports personalized treatment avenues. The ongoing evolution in AI methodology, particularly in relation to learning from multiple imaging timepoints, reflects a landmark shift that could soon be commonplace in hospitals worldwide, potentially transforming the landscape for pediatric cancer care.
Challenges in Implementing AI-Driven Risk Predictions
Despite the promising results of AI tools in predicting pediatric cancer recurrence, several challenges remain in their widespread implementation. Data privacy issues, the need for extensive validation across diverse clinical settings, and the integration of these tools into existing healthcare systems pose significant hurdles. Moreover, clinicians must be prepared to interpret AI-driven predictions and incorporate them into their clinical judgment responsibly.
Furthermore, while the initial findings are compelling, ongoing research is crucial for establishing guidelines about the optimal use of these AI tools in clinical practice. Addressing these challenges will require collaboration among healthcare providers, researchers, and regulatory bodies to ensure that AI-driven predictions are utilized effectively and ethically, ultimately enhancing the care provided to pediatric patients facing the complexities of cancer.
Future Directions in AI-Powered Pediatric Oncology
As researchers develop and refine AI tools for pediatric oncology, the future promises even more sophisticated applications, potentially transcending current limitations. The capacity for AI to analyze imaging data and predict cancer recurrence could extend beyond gliomas to other types of pediatric cancers. Innovations in algorithm development and machine learning techniques will likely diversify the applications of AI in medicine, enhancing accuracy and reliability.
Moreover, as clinical trials expand, data collected will provide deeper insights into the efficacy of AI in predicting not only the risk of recurrence but also the impacts that different treatment paths may have on long-term patient outcomes. By harnessing the power of AI, the pediatric oncology field stands to significantly improve how we approach treatment strategies and risk management in young patients, ultimately leading to more effective and personalized care.
The Role of Multi-Timepoint Imaging in Pediatric Cancer Care
Multi-timepoint imaging plays a pivotal role in the latest advancements in pediatric cancer care, especially concerning gliomas. By leveraging a series of MRI scans taken over time post-surgery, the AI models developed in recent studies have shown a dramatic increase in predicting cancer recurrence rates. This method allows for a comprehensive view of the patient’s condition, revealing crucial details that a single scan may overlook.
The importance of multi-timepoint imaging cannot be overstated; it empowers clinicians not only to monitor the progression of the disease more accurately but also to reassure families during the often stressful wait for follow-up assessments. As the technology surrounding multi-timepoint imaging continues to advance, it is likely that the integration of these insights into clinical practice will set new standards for monitoring pediatric cancer patients.
Interdisciplinary Collaboration: A Key to Advancements in Pediatric Cancer Prediction
Effective interdisciplinary collaboration is essential for maximizing advancements in pediatric cancer prediction, particularly in implementing AI technologies. The collaborative efforts between institutions like Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center have proven pivotal in gathering extensive data and refining AI models. This synergy illustrates the power of shared knowledge and resources in driving innovations that address clinical challenges in pediatric oncology.
As teams of experts from varying disciplines come together—combining specializations in AI, medicine, and oncology—they create a fertile ground for breakthroughs in patient care. Such collaboration is crucial for both enhancing the analytical capabilities of AI tools and ensuring these insights translate into practical applications in clinical environments, ultimately improving patient outcomes and fostering a healthcare ecosystem adept at navigating the complexities of pediatric cancer.
Frequently Asked Questions
How does AI pediatric cancer prediction improve the detection of relapse risk in children?
AI pediatric cancer prediction enhances the detection of relapse risk by utilizing advanced algorithms that analyze multiple brain scans over time. This approach, especially with techniques like temporal learning, allows for more accurate predictions by identifying subtle changes in radiographic images post-treatment, thus improving the management of pediatric glioma patients.
What role does temporal learning play in AI pediatric cancer prediction?
Temporal learning plays a crucial role in AI pediatric cancer prediction by enabling the analysis of sequential imaging data. It trains AI models to recognize patterns and changes in brain scans over time, significantly improving the accuracy of predicting pediatric cancer recurrence compared to traditional single-scan methods.
Can AI in medicine significantly enhance outcomes for pediatric brain tumor treatment?
Yes, AI in medicine can significantly enhance outcomes for pediatric brain tumor treatment by providing precise predictions about cancer recurrence. By analyzing multiple MRIs through temporal learning, clinicians can make informed decisions, potentially adjusting treatment plans based on the identified risks of relapse in pediatric patients with gliomas.
What is the accuracy rate of AI models in predicting pediatric cancer recurrence compared to conventional methods?
The AI models utilizing temporal learning have demonstrated an accuracy rate of 75-89% in predicting pediatric cancer recurrence, particularly for gliomas, significantly outperforming conventional methods which have around 50% accuracy, akin to random chance.
How can AI pediatric cancer prediction reduce the burden of follow-up imaging for patients?
AI pediatric cancer prediction can reduce the burden of follow-up imaging by identifying low-risk patients who may not require frequent MRIs. By accurately predicting relapse risk through advanced algorithms, healthcare providers can optimize diagnostic workflows and reduce stress for children and their families.
What potential benefits can AI offer in glioma risk assessment for children?
AI can offer considerable benefits in glioma risk assessment for children by providing a more reliable method for predicting which patients are at higher risk of tumor recurrence. This could lead to tailored treatment strategies, improved patient monitoring, and personalized care to enhance overall health outcomes.
What next steps are needed for implementing AI in pediatric cancer prediction in clinical settings?
Future steps for implementing AI in pediatric cancer prediction include conducting further validation studies across diverse clinical settings. Researchers aim to initiate clinical trials to assess the impact of AI-guided risk predictions on patient care, ensuring its effectiveness prior to widespread adoption in clinical practice.
How does AI analysis of longitudinal imaging impact the management of pediatric cancer patients?
AI analysis of longitudinal imaging profoundly impacts the management of pediatric cancer patients by providing comprehensive insights into tumor behavior over time. This method enables healthcare professionals to make proactive treatment choices, potentially enhancing the quality of care and improving patient prognosis.
| Key Points | Details |
|---|---|
| AI Tool Performance | AI tool demonstrates higher accuracy in predicting relapse risk in pediatric cancer than traditional methods. |
| Study Overview | Study published in *The New England Journal of Medicine AI*, involving 4,000 MRI scans from 715 pediatric patients. |
| Temporal Learning Method | AI model leverages multiple brain scans over time to improve predictions of cancer recurrence. |
| Prediction Accuracy | Achieved 75-89% accuracy in predicting recurrence of gliomas, compared to 50% for single images. |
| Future Applications | Research aims to initiate clinical trials to evaluate AI-guided predictions for patient care. |
Summary
AI pediatric cancer prediction has emerged as a transformative tool in the medical field, particularly in predicting relapse risks for pediatric cancer patients. Research conducted by Harvard researchers showcases the efficacy of an AI-based model that leverages temporal learning, analyzing multiple MRI scans from patients over time, leading to significantly improved accuracy in forecasting cancer recurrences. This innovation not only enhances predictive capabilities but also aims to optimize patient care through tailored treatment strategies, marking a critical advancement in pediatric oncology.