Predicting brain cancer relapse is becoming a critical focus in pediatric oncology, as advancements in technology reshape how we understand and manage the disease. A groundbreaking study from Harvard has revealed that an AI tool significantly outperforms traditional approaches in forecasting the risk of relapse in children suffering from gliomas, a type of brain tumor. The use of AI in pediatric oncology not only enhances the accuracy of glioma recurrence prediction but also alleviates the stress of frequent MRI scans that children and their families typically endure. By implementing innovative techniques such as temporal learning in AI, researchers can analyze a series of brain scans to identify subtle changes and improve brain tumor prognosis. This shift toward more reliable predictive methods marks an important step forward in pediatric cancer imaging and treatment, offering hope for better management strategies for young patients.
In the realm of pediatric cancer management, accurately forecasting the recurrence of brain tumors has emerged as a vital concern. Sophisticated artificial intelligence systems are now being employed to enhance detection methods, particularly for common brain tumors like gliomas, which may have varying rates of return. By harnessing techniques like sequential analysis of medical images, or what is referred to as temporal learning, researchers aim to offer improved insights into brain tumor outcomes. These innovative approaches not only focus on the cellular characteristics of tumors but also consider the dynamic changes in imaging over time, aiming to refine the prognosis for vulnerable pediatric patients. As the field evolves, the combination of technology and medical expertise holds promise for transforming how we approach brain cancer relapse predictions.
Understanding Brain Tumors in Pediatric Patients
Pediatric brain tumors, particularly gliomas, represent a significant challenge in oncology. Unlike adult brain cancers, which may have more established treatment protocols, pediatric brain tumors often present unique complications due to the patient’s developing brain and growing body. These tumors can vary widely in their aggressiveness and recurrence patterns, making individualized treatment strategies essential. Improper management or recurrence of these diseases can lead to devastating consequences, including serious neurological deficits and poor long-term outcomes.
It’s crucial for healthcare providers to go beyond conventional treatment plans and consider the specific biological and genetic factors contributing to each child’s brain tumor. This understanding is pivotal in helping doctors predict brain tumor prognosis better. Research is increasingly highlighting the importance of tumor profiling, which examines the molecular characteristics of gliomas, to tailor treatments that will minimize the risk of recurrence while maximizing the chance for a full recovery.
The Role of AI in Pediatric Oncology
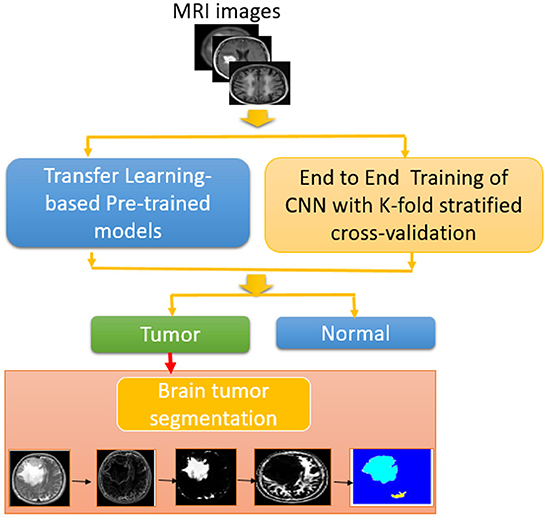
Artificial Intelligence (AI) stands at the forefront of transforming pediatric oncology. By employing machine learning algorithms, researchers can analyze vast datasets, including imaging and clinical outcomes, to discover patterns that may elude traditional analysis methods. AI tools are now able to process complex information from multiple sources, such as MRI scans and patient history, and predict glioma recurrence with remarkable accuracy. This predictive capability enhances clinical decision-making and gives families hope for better management of their child’s condition.
Several studies, including one from Harvard, emphasize how AI, particularly through techniques like temporal learning, is refining our approach to brain cancer prognosis. This specialized method utilizes a series of sequential brain imaging scans, teaching AI how tumor markers change over time. As a result, clinicians can gain insight into which patients are at higher risk and might benefit from more aggressive surveillance or treatment, ultimately improving the quality of care for young patients facing cancer.
AI in pediatric oncology not only optimizes current diagnostic methods but also opens the door to future innovations in treatment strategies, making it a game-changer in the field.
Predicting Brain Cancer Relapse Using Temporal Learning
Predicting brain cancer relapse is a critical aspect of managing pediatric gliomas. The innovative use of temporal learning allows AI models to analyze sequences of MRI scans to identify subtle changes that may indicate a potential return of the disease. Traditional predictive methods based on single imaging assessments often fail to provide reliable risk evaluations, hovering around 50% accuracy. In contrast, the temporal learning model demonstrated a significant leap in predictive capabilities, achieving accuracy rates between 75-89% for low- and high-grade gliomas.
With this approach, pediatric oncologists can monitor patients post-treatment with enhanced precision. The ability to detect precursors to relapse earlier could allow for tailored interventions, such as intensified surveillance or pre-emptive therapies for high-risk patients. This kind of forward-thinking initiative marks a shift toward personalized medicine in oncology, where treatments could become more proactive rather than merely reactive.
Advancements in Pediatric Cancer Imaging
Pediatric cancer imaging has undergone remarkable advancements, driven largely by technological innovations in AI and machine learning. Traditional MRI techniques are being enhanced with AI algorithms that refine image analysis, improving both the speed and accuracy with which clinicians can monitor tumor progression or regression. With the introduction of temporal learning models, the understanding of glioma behavior is evolving, allowing repeated imaging to develop a comprehensive view of tumor dynamics over time.
As researchers collect and analyze thousands of imaging studies, the goal is to enable rapid assessments that can lead to timely interventions. The collaboration between institutions like Mass General Brigham and Boston Children’s Hospital highlights the importance of large-scale data sharing and research partnerships in developing AI tools. This collective effort is essential in paving the way toward a more reliable imaging framework that aids in diagnosing and predicting the course of pediatric brain tumors.
Impact of AI on Treatment Strategies for Pediatric Gliomas
The integration of AI in predicting glioma recurrence not only enhances diagnostic accuracy but also significantly influences treatment strategies for pediatric patients. With more reliable predictions of relapse, oncologists can customize follow-up care, potentially reducing unnecessary repeat scans for low-risk cases and alleviating the emotional and physical burden on children and their families. Tailored treatment protocols can lead to better resource allocation and improved patient outcomes.
Moreover, precise identification of high-risk patients could prompt earlier intervention with adjuvant therapies designed to target residual tumor cells. By shifting from reactive to proactive management, healthcare providers can offer a new standard of care for pediatric patients grappling with brain tumors. This development showcases how the clinical application of AI can fundamentally change the landscape of pediatric oncology.
Collaborative Research Efforts in Pediatric Tumor Prognosis
The challenge of predicting pediatric brain cancer outcomes necessitates a collaborative approach involving multiple research institutions. The study showcased by Mass General Brigham, which included partnerships with prestigious entities such as Boston Children’s Hospital and Dana-Farber Cancer Institute, exemplifies how shared expertise can enhance research quality. These collaborations focus on pooling data from various pediatric patients to create a more significant impact in understanding tumor trends and recurrence risks.
Through such joint efforts, researchers can analyze extensive datasets, combining thousands of MRI scans and related patient information. This collective knowledge is invaluable in refining AI models and thus improving the prognostic capabilities for pediatric glioma patients. Collaborative projects emphasize the importance of interdisciplinary teamwork in advancing pediatric cancer care and providing hope to families navigating these dire circumstances.
Clinical Trials for AI-Powered Risk Assessment
As the landscape of pediatric oncology evolves with the introduction of AI, the need for clinical trials to assess the effectiveness of AI-powered risk assessments is paramount. Researchers are looking to test the AI tools developed through temporal learning in real-world clinical settings. These trials will establish whether predictions about glioma recurrence can lead to significant improvements in patient management, such as optimized imaging schedules or more effective treatment planning.
The outcomes of such clinical trials could redefine standard practices in how pediatric gliomas are monitored and treated. By confirming the reliability of AI predictions, these studies have the potential to enhance the quality of life for young patients, giving them tailored care that addresses their specific needs and risks. Ultimately, they could lead the way to broader acceptance and usage of AI technologies in the field of pediatric oncology.
Enhancing Patient Care Through Predictive Technologies
The integration of predictive technologies into pediatric oncology signifies a monumental shift in patient care. By utilizing advanced AI models capable of accurately forecasting glioma recurrences, clinicians can devise more proactive management strategies, thus ensuring better outcomes for children at risk. Enhanced prediction accuracy translates not just into timely interventions but also into improved psychological support for families, as they can have clearer expectations regarding their child’s health journey.
Moreover, reducing unnecessary imaging and hospital visits for low-risk patients can result in significant emotional and financial relief for families. These optimized care strategies foster a more supportive environment for young patients, allowing them to focus on recovery and connection rather than on frequent, anxiety-inducing medical appointments. Ultimately, the goal is to create a tailored approach that considers the child’s specific risk factors and medical history, enhancing not only clinical outcomes but overall quality of life.
Future Directions for AI in Pediatric Brain Tumor Management
Looking ahead, the future of AI in pediatric brain tumor management is promising. Continuous advancements in machine learning and AI technologies will undoubtedly lead to more refined predictive models capable of addressing the complexities of brain tumor behavior. Specifically, ongoing research into the interplay between genetic profiles of tumors and imaging results could yield groundbreaking insights, rendering oncologists capable of tailoring interventions based on individual patient biology.
The hope is that as these AI technologies evolve, they will provide comprehensive support tools for clinicians, fostering a more integrated approach to pediatric oncology. The continuous feedback loop created by implementing AI in clinical settings can enhance the data pool, leading to the development of even more sophisticated models. This represents a future where pediatric patients benefit not only from precise treatment regimens but also from a compassionate, patient-centered healthcare experience.
Frequently Asked Questions
How does AI in pediatric oncology improve predicting brain cancer relapse?
AI in pediatric oncology leverages advanced algorithms that analyze brain scans over time to detect patterns and changes that indicate the likelihood of glioma recurrence. By utilizing temporal learning, these AI tools can provide more accurate predictions compared to traditional methods that examine only individual scans.
What role does temporal learning in AI play in glioma recurrence prediction?
Temporal learning in AI enables the model to process multiple brain scans taken over time, allowing it to identify subtle changes that could signal a high risk of glioma recurrence. This innovative approach significantly enhances the accuracy of predicting brain cancer relapse compared to analyzing single images.
How effective is AI in predicting brain tumor prognosis after treatment?
The AI model developed through this research has shown an impressive accuracy rate of 75-89% in predicting brain tumor prognosis, particularly for gliomas, one year post-treatment. This represents a substantial improvement over traditional methods that typically achieve only about 50% accuracy.
What implications does AI have for pediatric cancer imaging in detecting relapse?
AI has the potential to revolutionize pediatric cancer imaging by enabling healthcare providers to monitor patients more efficiently. Through accurate risk predictions of brain cancer relapse, AI tools could help reduce unnecessary imaging for lower-risk patients while facilitating timely treatment for those at higher risk.
Are there any challenges in implementing AI for predicting brain cancer relapse in pediatric patients?
Yes, while AI offers promising advancements in predicting brain cancer relapse, researchers emphasize the need for further validation across various clinical settings before widespread clinical application. Ensuring the accuracy and reliability of the AI tools is crucial for enhancing patient care.
What makes glioma recurrence prediction challenging in pediatric patients?
Predicting glioma recurrence in pediatric patients is challenging due to the variable nature of the tumors and the fact that many can be cured with surgery alone. The inability to accurately identify those at highest risk of relapse results in prolonged and stressful follow-up imaging processes.
How could AI-informed risk predictions change the management of pediatric brain cancer patients?
AI-informed risk predictions could lead to more personalized management strategies for pediatric brain cancer patients, enabling clinicians to tailor follow-up imaging schedules or initiate targeted therapies for patients identified as high-risk for recurrence.
| Key Point | Details |
|---|---|
| AI Tool Development | An AI tool developed by a Harvard collaboration is showing superior results in predicting pediatric brain cancer relapse. |
| Study Focus | The study focuses on pediatric gliomas that, while treatable with surgery, have varying relapse risks. |
| Predictive Accuracy | The AI tool achieves 75-89% accuracy in predicting relapse, outperforming traditional methods that had about 50% accuracy. |
| Temporal Learning Technique | The AI utilizes a novel temporal learning technique to analyze multiple scans over time, improving prediction reliability. |
| Future Steps | The researchers aim to conduct clinical trials to assess the practical application of their findings in patient care. |
Summary
Predicting brain cancer relapse has become more precise with the introduction of an advanced AI tool that significantly improves forecast accuracy for pediatric glioma patients. By analyzing multiple brain scans over time, this innovative approach enables healthcare providers to identify children who are at high risk of recurrence, potentially transforming their care strategy. Continued research and clinical trials will further validate the benefits this AI tool could offer, paving the way for tailored treatment plans and a better understanding of pediatric brain cancer dynamics.